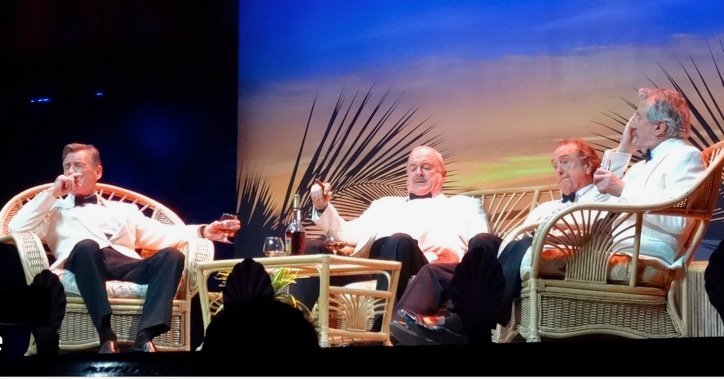
Four Yorkshiremen of the apocalypse
BBC image
You were lucky!!
You may remember the Monty Python inspired sketch about the four men from Yorkshire who reminisce about their upbringing. As the conversation progresses, they outdo one another with increasingly absurd accounts of their deprived childhoods. "We had to live in a cardboard box?" ... "A cardboard box? You were lucky! We lived for three months in a rolled-up newspaper in a septic tank."
Like anyone who has worked for a long time in a profession, there is a similar tendency to compare now with then; for Doctors it goes something like: ‘it wasn’t like that in my day’, or ‘I worked a 1 in 3 rota for 5 years’ or ‘we didn’t have people to take blood for us back then’.
Yet despite many improvements in work conditions over the past 30 years, levels of stress and burnout among doctors are worse than ever. In the past, doctors faced intense rotas, fewer senior staff, and uncertain career progression with training posts often just lasting 6-12 months. Some of the stresses were reduced by implementing the European Working Time Directive (EWTD) to limit working hours and improve rest periods. Specialist training is more structured without the need to be permanently looking for the next post. There are undoubtedly more clinicians at senior levels. However the the mental health crisis among clinicians has persisted and even worsened.
So what has changed?
Within the NHS the nature of workplace support and organisational culture has changed. The NHS battles with staff shortages, high workloads, and administrative inefficiencies, which contribute to chronic stress. The NHS Staff Survey 2023 showed high levels of burnout among clinical staff; astonishingly nearly 35% of medical and dental professionals reporting burnout. These pressures are added to by the emotional toll of patient care, increased public scrutiny, and the increasing complexity of healthcare delivery.
What is the organisational role?
Support from leaders and managers is crucial. Many, if not most, Doctors feel that they are inadequately supported, particularly in dealing with high workloads and protecting their health and well-being. The lack of effective feedback mechanisms and the pressure to meet service demands often leaves doctors feeling undervalued and unsupported, exacerbating burnout.
The NHS has been criticised for its treatment of whistleblowers - staff who raise concerns about patient safety, governance, or misconduct. The recent high-profile case of Dr. Maxwell McLean, former Chair of Bradford Teaching Hospitals NHS Foundation Trust, has brought renewed attention to the adequacy of protections for those who speak up. If you cannot speak up when things are going wrong, the sense of futility and demoralisation increases.
What do the Public think?
Despite the percetion amongst Doctors, surveys continue to show that Doctors are among the most trusted professionals. There seems to have been a subtle decline in trust in nurses and hospital managers, possibly influenced by high-profile scandals and sensationalised media coverage of care failures. The public used to be been sympathetic, understanding that errors are often unintentional and part of the human element in medicine. Today, there has been a shift, with mistakes viewed more critically. This increases clinician frustration and provokes a sense of ineffectiveness. You only have to look at Social Media (Including LinkedIn) to find examples of medical failures, which are not, unfortunately, always presented in a fair or balanced way.
Can coaching help?
Interventions like coaching are part of the broader strategy to combat burnout. Coaching develops resilience, improves work-life balance, and assists in navigating organisational challenges. It helps the Doctor to cope; however the NHS also needs to address staffing shortages, rota design, administrative burdens, and (crucially) organisational culture. There is strong support for the view that organisational interventions, combined with individual support like coaching, can significantly reduce burnout.
Conclusion
The rise in stress and burnout among doctors, despite advancements in work regulations and support structures, reflects deep systemic issues within healthcare organisations and public perceptions. Improving organisational support, fostering a culture of open communication and treating whistleblowers as allies rather than enemies. The NHS must implement effective targeted interventions like coaching, whilst addressing workload and staffing challenges. Only then can we ensure the well-being of clinicians and the sustainability of healthcare services.
If you are a health professional who is struggling to manage the many demands on your professional life, if you feel unsupported and undervalued, or if you feel you are no longer on the same page as your employers, why not consider seeking help from an Executive Coach. You can book a free no obligation 30 minute on-line conversation with me here. If I am not the right Coach for you, I will recommend somebody else who might be.
Please check my website and sign up to my mailing list if you want to receive posts like this directly to your inbox.